 Businesses Act, 1991 (Act No. 71 of 1991)
Businesses Act, 1991 (Act No. 71 of 1991)
R 385
Pharmacy Act, 1974 (Act No. 53 of 1974)Board NoticesPrimary Care Drug Therapy Pharmacist (PCDT)Part 2 : Competency Standards for a Pharmacist providing Primary Care Drug Therapy |
ACRONYMS
| DOH | Department of Health |
| EML | Essential Medicines List |
| PCDT | Primary Care Drug Therapy |
| PHC | Primary Health Care |
| SA | South Africa |
| SAPC | South African Pharmacy Council |
| STG | Standard Treatment Guidelines |
DEFINITIONS
Behavioural statement: are statements which describe the activity or outcomes prescribers should be able to demonstrate.
Competency: A quality or characteristic of a person related to effective or superior performance. Competency consists of aspects such as attitudes, motives, traits, and skills.
Domain: Represents an organised cluster of competencies within a framework and the domains, with associated competencies.
| 1. | INTRODUCTION |
Pharmacists have a broad scope of practice which allow them to render additional services provided they meet the prescribed minimum requirements. Primary Care Drug Therapy (PCDT) is one of the services that a pharmacist may provide upon completion of a supplementary training course with an accredited higher education institution. On completion of the course, a certificate of completion should be registered with the South African Pharmacy Council (SAPC) prior to submission of an application for a PCDT permit with the Department of Health (DoH). Following the issuing of the permit by the DoH, Pharmacists are required to record the permit with the SAPC. The permit will authorise a pharmacist to diagnose, prescribe and administer medicine for selected conditions in line with Primary Health Care (PHC) level Standard Treatment Guidelines (STG) and Essential Medicine List (EML).
| 2. | BACKGROUND |
The main goal of extending prescribing to pharmacists is to improve patient care without compromising patient safety, increase access to health care services, increase patient choice, make better use of the skills of health professionals and contribute to the introduction of a more flexible team working in primary health care settings. Pharmacists are expected to apply the principles of pharmaceutical care in providing PCDT services. Pharmaceutical care is a patient centred, outcomes orientated pharmacy practice that requires the pharmacist to work in conjunction with the patient and the patient's other healthcare providers to promote health, to prevent disease, and to assess, monitor, initiate and modify medication use to assure that medicine therapy is safe and effective. The competency standards and scope of practice of PCDT pharmacist prescriber will enable them to practise and develop as prescribers and assist in meeting the health care needs of the country in line with the PHC EML and STG.
| 3. | DEVELOPMENT OF COMPETENCY STANDARDS FOR PCDT PHARMACIST |
The following documents form the basis for the development of competency standards for PCDT pharmacist:
| • | PCDT pharmacist qualification and scope of practice |
| • | The scope of practice and competency standards for pharmacists Competency standards for a PCDT pharmacist have been developed to supplement the approved pharmacist competency standards, in advanced level of practice. Comparison of international competency standards for prescribing pharmacists was also useful to give guidance in determining both the domains and the standards. |
These competency standards were developed to supplement the competency standards for pharmacists at an advanced level of practice pertaining to PCDT.
| 4. | SUMMARY OF COMPETENCY STANDARDS FOR PCDT PHARMACIST |
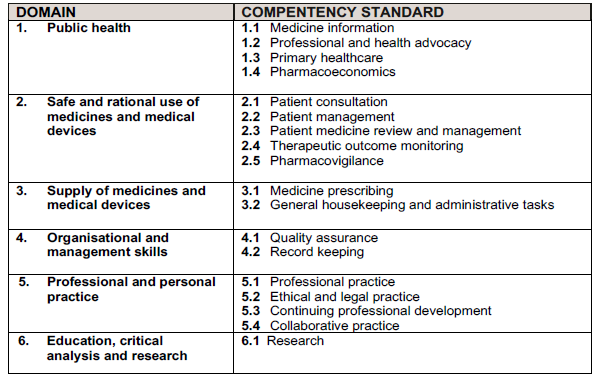
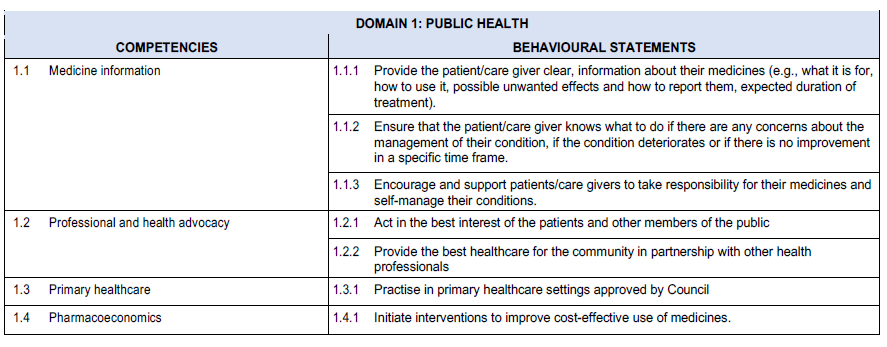
DOMAIN 1: PUBLIC HEALTH
INTRODUCTION
Domain 1 covers public health and includes competencies that are required in both the public and private healthcare sectors to promote health and wellness through the provision of healthcare information and education to the public and other members of the healthcare team. The provision of medicines and healthcare information and education forms an integral part of the scope of practice of a pharmacist. The availability of specialised pharmaceutical knowledge at all levels of care, including primary healthcare (PHC), is an important component for the delivery of effective and efficient pharmaceutical services. The domain covers competencies that are required to promote health, promote and monitor adherence.
The public health domain competencies are:
| 1.1 | Medicine information |
| 1.2 | Professional and health advocacy |
| 1.3 | Primary healthcare |
| 1.4 | Pharmacoeconomics |
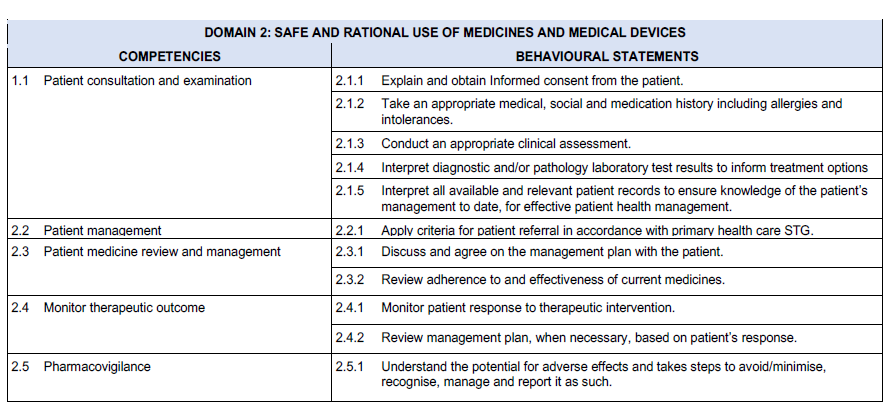
DOMAIN 2: SAFE AND RATIONAL USE OF MEDICINES AND MEDICAL DEVICES
INTRODUCTION
Domain 2 covers competencies that are required to ensure safe and rational use of medicines and administration devices, in this domain effective verbal and non-verbal methods of communication with patients are essential competencies.
The competencies required in the domain for the safe and rational use of medicines are:
| 2.1 | Patient consultation |
| 2.2 | Patient management |
| 2.3 | Patient medicine review and management |
| 2.4 | Monitor therapeutic outcome |
| 2.5 | Pharmacovigilance |
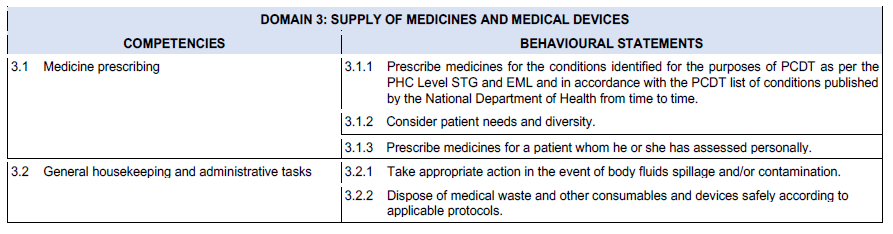
DOMAIN 3: SUPPLY OF MEDICINES AND MEDICAL DEVICES
INTRODUCTION
Domain 3 includes competencies required to address the supply of medicines to patients, the behavioural statement in this domain includes prescribing of medicines.
The competencies required in the domain for the safe and rational use of medicines are:
| 3.1 | Medicine prescribing |
| 3.2 | General housekeeping and administrative tasks |
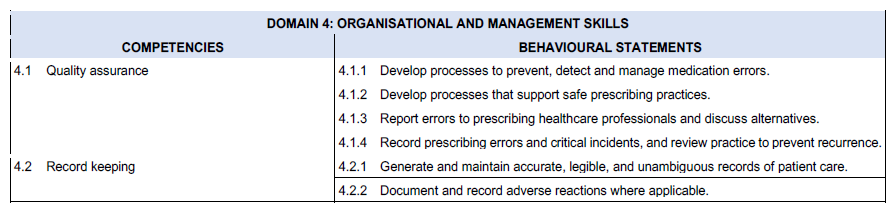
DOMAIN 4: ORGANISATIONAL AND MANAGEMENT SKILLS
INTRODUCTION
Domain 4 includes competencies required to ensure effective and efficient delivery of PCDT services including amongst other behavioural statements development of the required processes and procedures.
The competencies required are:
| 4.1 | Quality assurance |
| 4.2 | Record keeping |
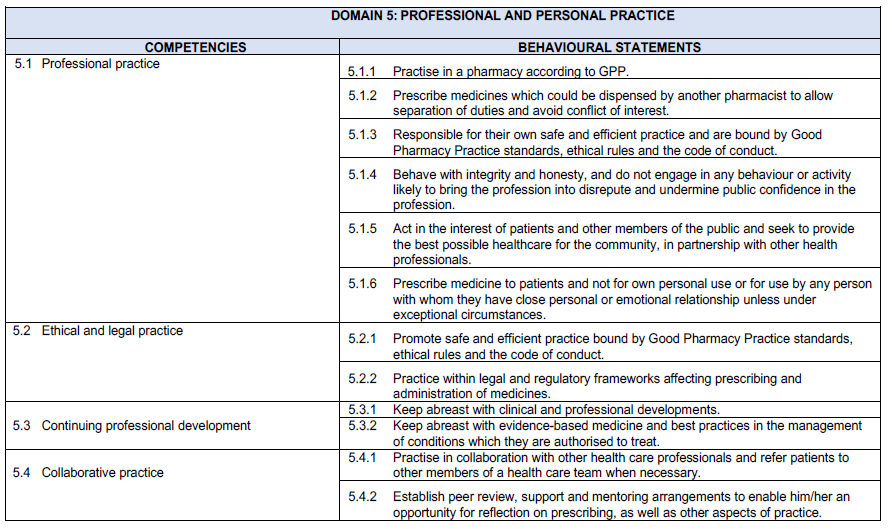
DOMAIN 5: PROFESSIONAL AND PERSONAL PRACTICE
INTRODUCTION
Domain 5 includes behavioural statements that focuses on professional practice, code of conduct and adhering to legal requirements and ability to work collaboratively with other healthcare professionals.
The competencies required are:
| 5.1 | Professional practice |
| 5.2 | Ethical and legal practice |
| 5.3 | Continuing professional development |
| 5.4 | Collaborative practice |
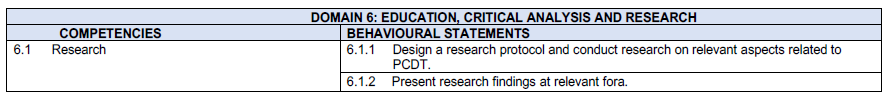
DOMAIN 6: EDUCATION, CRITICAL ANALYSIS AND RESEARCH
INTRODUCTION
Domain 6 includes the behavioural statements relating to education and training, critical analysis and research. Pharmacists should participate in practice-based research. The research may include investigations into prescribing practices, patterns of medicine usage, evaluation of medicine use, the monitoring of adverse reactions, the benefits of the pharmacist’s advisory role, computerised data handling, health economics, legislation, and aspects of abuse and irrational use of medicines. Practising pharmacists are increasingly participating in health systems and quality improvement research, which must be encouraged as a means of providing databases and information for future policy, guidelines and practice development. Such research is often conducted in collaboration with other healthcare providers.
The education, research and critical analysis competencies are:
| 6.1 | Research |
| 5. | REFERENCES |
https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Prof essional%20standards/Prescribing%20competency%20framework/prescribing-competency-framework.pdf.
Royal Pharmaceutical Society. A competency framework for all prescribers. July 2020.
South African Pharmacy Council Board Notice 122 of 2011. Scope Of Practice and Qualification for Authorised Pharmacist Prescriber Published 01 July 2011.
South African Pharmacy Council Board Notice 59 of 2018. The Pharmacy Act (53/1974): Competency Standards for Pharmacists in South Africa. Published on 11 May 2018.